Check if you really need antibiotics
PETALING JAYA – “There’s data everywhere in the world to show that the more you use antibiotics, the higher the bacterial resistance towards antibiotics,” said Sungai Buloh Hospital Infectious Disease head Datuk Dr Christopher Lee.
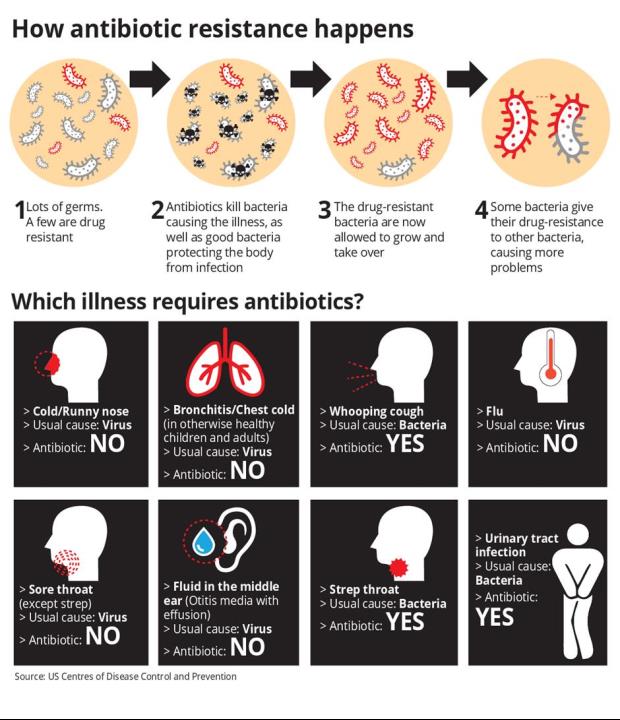
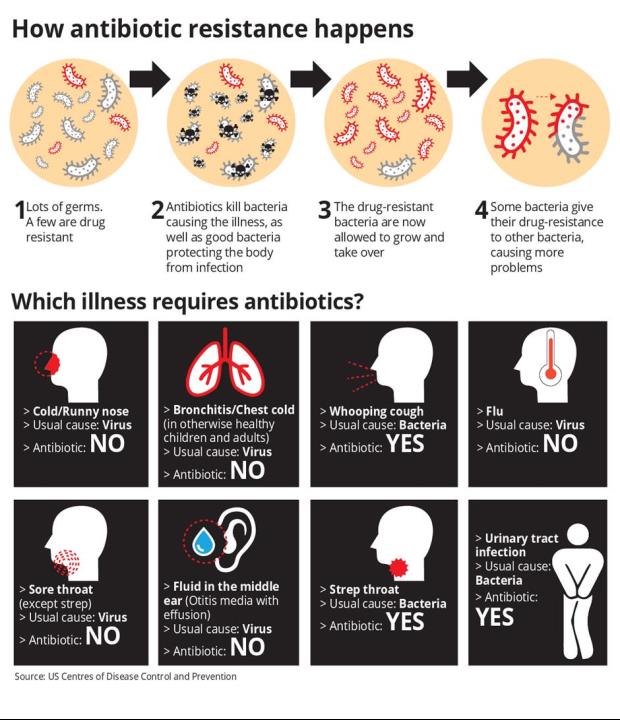
Antibiotics are only useful for bacterial infections, not viral infections.
Dr Lee explained that viruses are the most common cause of infections, and that antibiotics have no direct impact on them.
“The most common illness that anyone gets as they grow up would be the common cold.
“You will develop sniffles, have a little bit of fever, you feel miserable for a few days, your voice sounds croaky, but after that you get better. All these common cold symptoms we can lump it under the broad category of upper respiratory tract infections (URTI),” he said.
He shared that 85 per cent to 90 per cent of URTI are due to viruses, hence there is no need to consume antibiotics because of it.
“I want to remind people that fever doesn’t necessarily mean infection, and infection doesn’t always arise from bacteria.
“Even for bacterial infections, only some of them require the use of antibiotics. Some are so mild that you can recover by yourself,” he said.
“For example, a pimple is an infection of your pore. But do you need antibiotics? No. With good hygiene, it will clear by itself.”
He explained that not every illness requires the use of antibiotics.
“Most sore throats tend to be due to viruses. With a normal viral infection, by day three or so, the fever has started coming down. If so, as a general rule of thumb, you do not need antibiotics,” he said.
“If you cough when you contract an URTI, it can take up to 10 days for the cough to subside. Taking antibiotics doesn’t make it go away faster, because the throat takes time to recover from that viral infection,” he said.
Dr Lee added that patients should look at the severity of the symptoms rather than their duration as a guide to whether it is a bacterial infection.
He said if the cough is persisting but its symptoms are not getting any worse, it may not be a cause of concern.
“These suggestions are for patients who don’t have any other illnesses. However, if you are on chemotherapy for instance, or if you’re on steroids, this advice doesn’t hold for you,” he said.
Over time, Dr Lee warned, the continued overuse and misuse of antibiotics may lead to antibiotic resistance.
“One common bacteria called streptococcus pneumoniae, which causes chest and throat infection, is treated by a common class of drugs called macrolide. Examples of this class would be erythromycin and azithromycin.
“In the past, up to 90 per cent of this bacteria will be killed by macrolide. Now the sensitivity levels have dropped. The original resistance level of about 10 per cent has now been increased to about 38 per cent over the last 10 years,” he noted.
He said that it is disconcerting that older antibiotics are no longer as effective, especially as the development of newer antibiotics has slowed down.
“In the past, we were able to get away with bacteria developing resistance towards antibiotics because there’s always some new antibiotic that will come along,” he said. “But for the last 10 to 15 years, the pipeline is getting dry. There are very few new classes of drugs.”
Thus, he said that the efforts to preserve the effectiveness of the antibiotics already existing have become more urgent.
“We cannot say we should ban antibiotics, but we need to use them at the right time, with the right dosage, and for the right duration,” he said.
For this, patients and doctors need to ask themselves whether it’s absolutely necessary to start a course of antibiotics.
“I’m not asking patients to fight with their doctors or second-guess them, but it’s okay to have a conversation with your doctor and to ask whether antibiotics are needed,” he said.
He said that doctors may be prescribing antibiotics unnecessarily because patients demand them.
“We know some doctors are driven by commercial aspects. Let’s say a doctor doesn’t give a patient antibiotics. The upset patient may go to the next clinic and get the antibiotics, so the doctor loses the patient,” he said.
He also said that doctors may feel worried that they may have missed out on seeing the signs of a bacterial infection, and deemed it best to prescribe antibiotics just in case.
However, he recommended that doctors issue a deferred antibiotic prescription instead. “In the UK, the doctors practise this. They do not dispense the medicine, the patients have to collect it from the nearest pharmacy.
“When doctors issue a deferred antibiotic prescription, a patient will wait and see if in the next two days they start feeling worse. If they do, only then can they collect the antibiotics and start the course of treatment,” he said.
He said it’s possible to implement this system on a local level in Malaysia, but patients may feel that it’s troublesome to return to the doctors to collect their antibiotics a few days later.
“Patients should understand that doctors are not doing this to make it more troublesome for them,” he said.
“Patients may also worry about doctors charging consultation fees again. Now I’m not saying that doctors will or won’t do that, as a lot depends on the doctor’s intention to reduce the use of antibiotics.
“It could also be that the doctors are not aware that antibiotics are not necessarily suitable. Maybe their understanding of how to treat a sore throat is different or out of date,” said Dr Lee.
He explained that there are clinical scores, such as the Centor score, for doctors to determine whether an infection is bacterial or viral.
“For example, the most common illness is sore throat. There are clinical scores to check whether the symptoms are attributed to bacterial infections.
“These scores are not foolproof but at least it’s better than immediately prescribing antibiotics.”
Dr Lee also advised against bad consumption habits, such as not completing the course of antibiotics prescribed or sharing antibiotics with other family members.
“Your sore throat may have a different cause than another person’s sore throat. The symptoms may generally be alike, but antibiotics are not a one-size-fits-all solution,” he said.
“In this case, sharing is clearly not caring.”
Published at Mon, 06 Nov 2017 01:34:34 +0000